Why Rainbow Babies Are So Special
Rainbows have always been a symbol of peace, hope and positivity. We look for rainbows after a storm - when the rain stops and the sun breaks through the clouds and shines bright light down on the earth. “Rainbow babies” are those who are conceived after a loss – these babies are so special because they represent a bright light of hope and joy that can help families recover from a challenging time in their lives.
Whether you’ve experienced a loss yourself, or you’ve stood by a mother/daughter/sister/friend and supported her on this difficult journey, it’s important to recognize that families are not alone in this process. According to Mayo Clinic, approximately 10-20% of known pregnancies result in a loss. It is normal to grieve and go through a variety of emotions when making the decision to try again. We’re honored to have cultivated such a supportive, loving community of women who are willing to share their real, raw, emotional stories in an effort to help one another.
In honor of the women who’ve experienced a loss, and all of the rainbow babies who represent healing and love, we’d like to celebrate you by sharing some real stories (and adorable photos!) from the Glow community!

“Our rainbow baby girl after two miscarriages 😍🌈” - Glow App user, Holly

“In 2017, I had a little boy at 24 weeks, his name was Brysen. He was one pound seven ounces. I had a 40% placental abruption and was bleeding out, and the doctors were forced to deliver him by emergency c-section. I had three blood transfusions, two platelet transfusions. He fought three long and very hard days before losing his battle. The only time I got to hold my first baby boy, was the moment he took his last breath in my arms. His breathing was so labored, it almost seemed as though he waited to get into my arms. I held him for about twenty seconds before my beautiful little man took his last breath, almost as a sigh of relief. In March of 2019, I delivered my beautiful rainbow baby. He is the light of our life, and I am so happy I got my beautiful rainbow, even after the hellacious storm.” - Glow App user, Laney

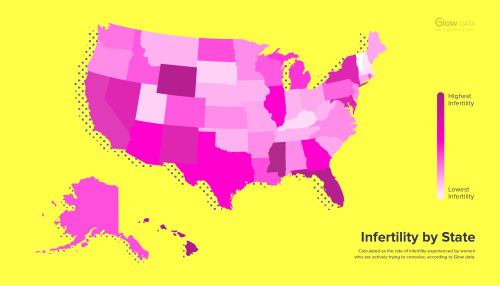
“Our sweet William James. We struggled with unexplained infertility for six years. After every treatment I finally gave up and just wanted to focus on traveling and just being with my husband. Three months later, In July of 2018, we found out we were expecting our rainbow. He was born 3/13/19 🌈” - Glow App user, Megan

“This is Fox! We had one loss at twelve weeks and a few months later got pregnant with him…and here he is now at age two eating rainbow sprinkles😂” - Glow App user, Ashley

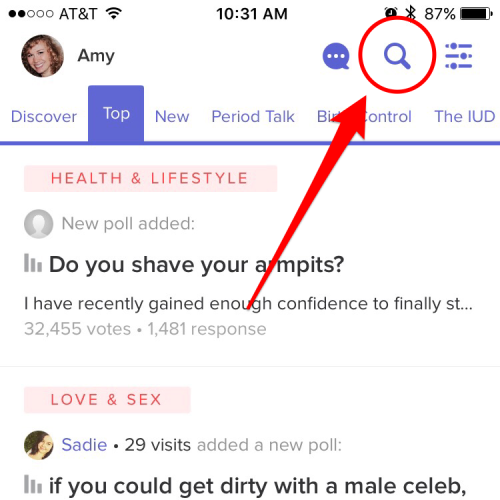
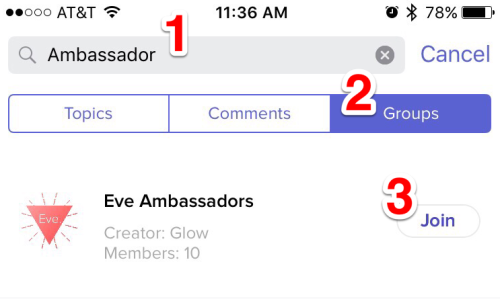
“Your app helped me get pregnant with my rainbow baby. She’s our greatest blessing AND we are due with our second baby girl in August! Thank you so much!” - Glow App user, Kimberly

“This is my Sweet Lyla Grace. Being pregnant for the first time ever I miscarried one week after my birthday. I was shattered. I’d never hold that baby in my belly or arms, but I’ve always held them in my heart. I was truly blessed to fall pregnant two months later with my rainbow baby. I remember feeling half on cloud 9 and half so scared my whole pregnancy that something would happen. No matter what I tried I was too scared to be happy. If I could tell myself back then everything happens for a reason I would. My beautiful daughter was born and she is the best thing that’s ever happened to us. She just turned one last week and now I’m six and half months pregnant with her sister! She will always be my saving grace and my rainbow after the storm.” - Glow app user, Becca
A huge thank you from the Glow team to everyone in our community for sharing your beautiful, inspiring stories!