Insurance and twins
U.S. mom here:
Did your insurance stop covering routine things for your twins simply because it was twins?
My insurance is supposed to cover routine prenatal care at 100%. That’s ultrasounds, blood work with routine screening, and office visits. Checked before we got pregnant and checked again now.
Well, I had my 20 week anatomy scan in January. Same thing you’d have done with a singleton pregnancy.
I’m now getting an about $750 bill for this. And they’re saying simply because it’s twins all the sudden we’re magically going to be paying until our deductible is reached instead of being covered at 100%. Twins gets billed as “diagnosis” which all the sudden puts me at not covered. Insurance person said “it’s how it’s billed...”
Has anyone else ran into this?? $750 a pop for an ultrasound and I’m supposed to go to MONTHLY ultrasounds now... our deductible in network is $15,000! Our insurance is not cheep per month either! I’m absolutely freaking out. My next ultrasound is supposed to be the 24th and I’m contemplating not going to it!! This is horrible.
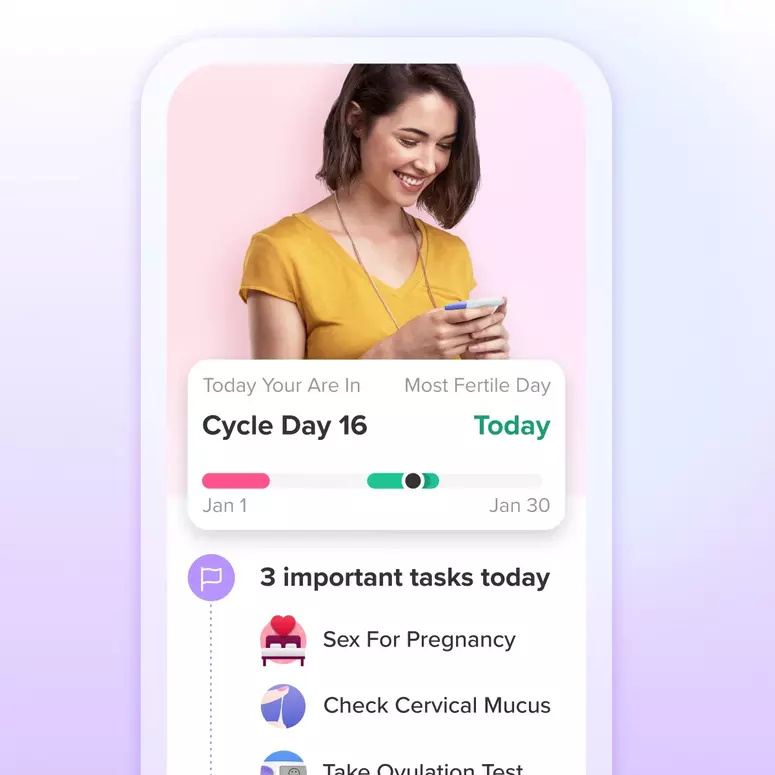
Achieve your health goals from period to parenting.