Progenity
So my ob office does Progenity genetic testing. I called Progenity to ask if they use my insurance and they said yes but I'll have to call my insurance. So I did and they said they pay for it as long as they send something to them. Not sure if they meant my ob or Progenity. I asked my ob and they said they don't send anything to my insurance they either pay or don't. They said they can write up a Test Requisition Form and send it to Progenity and Progenity deals with insurance using their codes or what not. Does anyone possibly know if insurance would still cover it if Progenity just sends them the bill or does my ob need to send whatever to get pre authorization. Anyone work for insurance and know what I'm talking about? I'll call tomorrow but just curious.
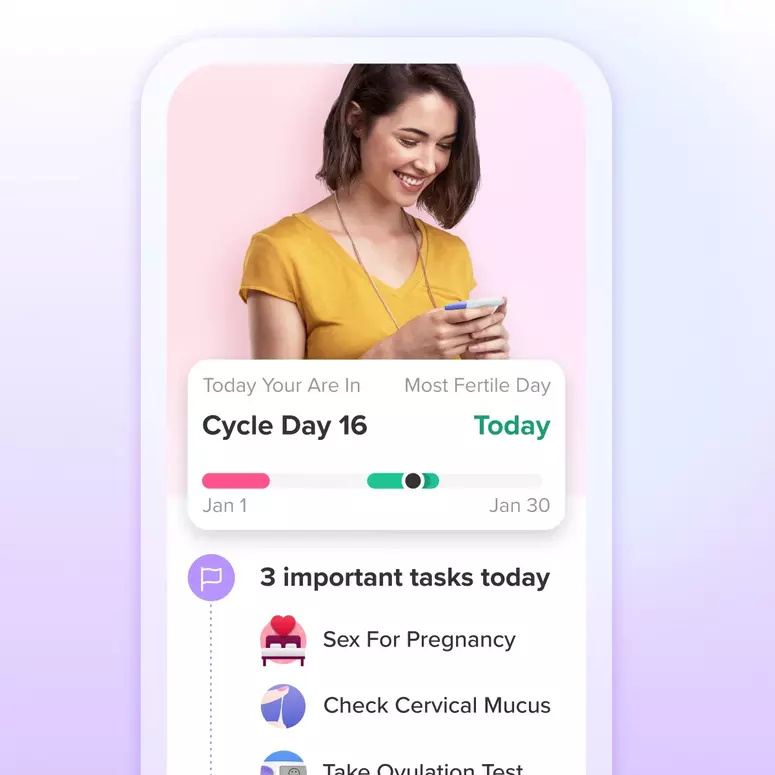
Achieve your health goals from period to parenting.