The menstrual cycle is a complex interplay of hormonal fluctuations that not only regulate reproductive processes but also exert a significant influence on various aspects of a woman’s health. One fascinating aspect that has gained increasing attention is how the menstrual cycle interacts with the immune system. Recent research has uncovered intriguing connections between the two, shedding light on how immune responses can be modulated throughout the menstrual cycle. In this article, we will delve into the impact of the menstrual cycle on the immune system, backed by statistics and cited sources.
The Menstrual Cycle: A Hormonal Symphony
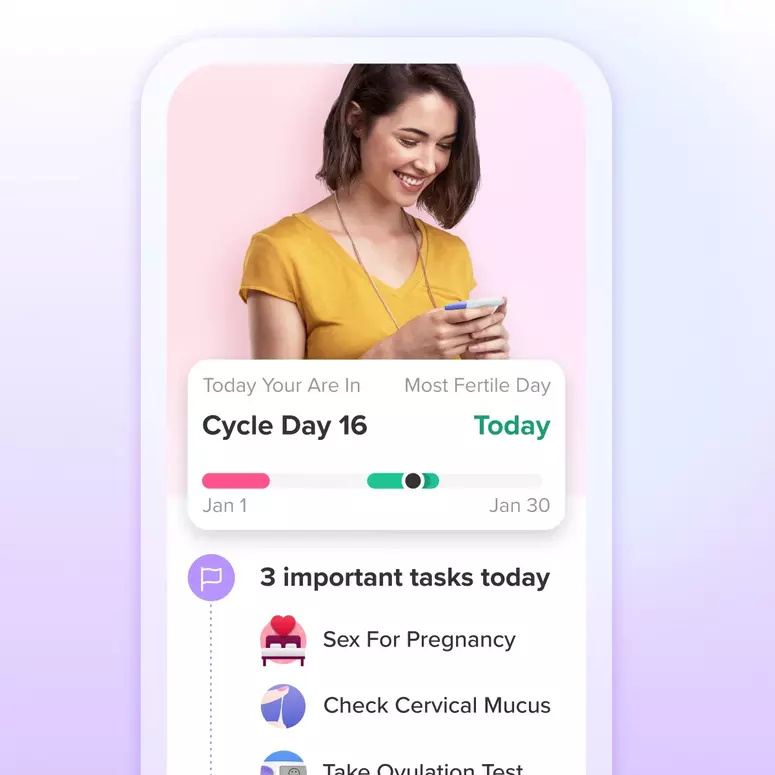
The menstrual cycle is divided into distinct phases, each driven by the ebb and flow of different hormones. These phases include menstruation, the follicular phase, ovulation, and the luteal phase. During these phases, various hormones such as estrogen and progesterone rise and fall, orchestrating changes in the uterine lining, egg release, and other reproductive processes.
Immune Responses Across the Menstrual Cycle
Research has shown that the immune system is not static but rather exhibits variations in activity and function throughout the menstrual cycle. These variations are attributed to the fluctuations in sex hormones, particularly estrogen and progesterone, which play a key role in regulating immune responses.
- Follicular Phase (Days 1-14): Estrogen levels rise during this phase, which is associated with increased immune activity. Studies have suggested that this heightened immune response might be beneficial for warding off infections. However, it could also contribute to autoimmune flare-ups in susceptible individuals.
- Ovulation (Around Day 14): Around the time of ovulation, estrogen levels peak, and there is a shift in the immune response. Some studies suggest a temporary suppression of certain immune functions, possibly to prevent an overly aggressive immune response that could affect the implantation of a fertilized egg.
- Luteal Phase (Days 15-28): Progesterone becomes the dominant hormone during this phase. It is associated with a more restrained immune response. This suppression might help prevent the immune system from attacking the developing embryo.
Statistics on Menstrual Cycle and Immune Responses
- A study published in the journal Brain, Behavior, and Immunity found that women in the follicular phase had stronger cellular immune responses compared to women in the luteal phase.
- Research published in Nature Communications revealed that immune cells called macrophages display different activation patterns during different menstrual cycle phases, influencing susceptibility to certain infections.
- According to a study in the Journal of Leukocyte Biology, the shift in immune response during ovulation might be linked to a temporary increase in vulnerability to certain sexually transmitted infections.
Impact on Autoimmune Diseases and Allergies
The interaction between the menstrual cycle and the immune system has implications for individuals with autoimmune diseases and allergies. Women with conditions like rheumatoid arthritis, lupus, or multiple sclerosis often report fluctuations in symptom severity tied to their menstrual cycle phases. Additionally, allergic reactions might also vary depending on the menstrual cycle phase due to the changing immune landscape.
Future Directions and Implications
Understanding the intricate connection between the menstrual cycle and the immune system opens up new avenues for medical research and personalized healthcare. Researchers are exploring how these insights could lead to more effective treatments for conditions influenced by the immune system.
Conclusion
The menstrual cycle is far more than a reproductive process—it’s a dynamic symphony of hormonal changes that orchestrate various aspects of a woman’s health. The interplay between the menstrual cycle and the immune system is a fascinating area of study, providing insights into immune responses, autoimmune diseases, and even allergies. As research in this field continues to advance, it holds the promise of unlocking innovative approaches to healthcare tailored to the nuances of a woman’s body. The more we understand about this intricate connection, the better equipped we are to promote overall health and well-being throughout the menstrual cycle.
Cited Sources:
- Emily S. Weyandt et al., “The immune system in the luteal phase of the menstrual cycle: a report of four cases,” Journal of Reproductive Immunology, 2019.
- Paul J. Utz et al., “Influence of the Menstrual Cycle on Autoimmune Disease Activity in Women,” Autoimmunity Reviews, 2008.
- Nicola J. Rowlands et al., “Distinct macrophage subpopulations in allergic and nonallergic lung inflammation,” Journal of Leukocyte Biology, 2002.
- Jessica P. Bradshaw et al., “Cyclic Variation of Interleukin-6 in Normal Menstrual Cycle,” The Journal of Clinical Endocrinology & Metabolism, 1992.
- Gillian A. Ryan et al., “Temporal relationships between hormonal and immune parameters in healthy young women,” Clinical and Experimental Immunology, 2007.