What is Menopause?
Menopause is when your periods stop permanently, and you can no longer get pregnant. You have reached menopause only after it has been a full year since your last period. This means you have not had any bleeding, including spotting, for 12 months in a row. Menopause can happen in the 40s or 50s. But the average age is 51 in the United States. After menopause, your ovaries make very low levels of the hormones called estrogen and progesterone. These low hormone levels can raise your risk for certain health problems.
Menopause is natural. But the physical symptoms, such as hot flashes, and emotional symptoms of menopause may disrupt sleep, lower energy or affect mood. There are many treatments, from lifestyle changes to hormone therapy.
Perimenopause: The Transition Phase
Perimenopause, also known as the menopausal transition, is the period leading up to menopause. It can begin several years before the final menstrual period, often in a woman’s 40s or even 30s. During the transition, the amount of hormones your ovaries make varies. Perimenopause can last 2 to 8 years. The average is about four years. During perimenopause, hormone levels fluctuate significantly, leading to a range of symptoms.
Common Symptoms of Perimenopause and Menopause
The decline in estrogen and progesterone during perimenopause and menopause can trigger various physical and emotional changes, including:
- Changes in menstruation: Irregular periods, changes in flow, and skipped periods are common during perimenopause.
- Hot flashes: Sudden feelings of warmth, often accompanied by sweating and flushing.
- Night sweats: Hot flashes that occur at night, disrupting sleep.
- Sleep disturbances: Difficulty falling asleep or staying asleep.
- Vaginal dryness: Thinning and drying of the vaginal tissues, leading to discomfort during intercourse.
- Mood changes: Irritability, anxiety, depression, and mood swings.
- Changes in libido: Reduced sexual desire.
- Cognitive changes: Difficulty concentrating, memory problems, and “brain fog.”
- Bone loss: Decreased estrogen levels can lead to osteoporosis, increasing the risk of fractures.
- Changes in cholesterol levels: Increased risk of cardiovascular disease.
- Weight gain: Changes in metabolism can contribute to weight gain, particularly around the abdomen.
When to see your healthcare professional
It’s essential to consult a healthcare professional to discuss any concerns or symptoms related to perimenopause or menopause that are worrying you. They can provide personalized advice, recommend appropriate treatments, and monitor overall health. Open communication with your doctor can help you navigate this natural transition with greater ease and well-being.
Several strategies can help manage symptoms and improve quality of life during this transition:
Lifestyle modifications
Managing menopausal symptoms effectively involves a holistic approach. Regular exercise not only reduces hot flashes but also enhances mood and preserves bone density. A balanced diet, emphasizing fruits, vegetables, whole grains, and calcium, provides essential nutritional support. Stress management techniques, such as yoga, meditation, and deep breathing exercises, can effectively regulate mood swings and anxiety. Finally, prioritizing adequate sleep through a consistent schedule and a calming bedtime routine is crucial for improving overall sleep quality.
Hormone therapy (HT)
Hormone therapy (HT) for menopause involves the use of medications containing female hormones to replace those the body no longer produces during and after menopause. This treatment aims to alleviate common symptoms such as hot flashes, night sweats, and vaginal dryness, and may also offer benefits for bone health. However, HT carries potential risks, including an increased risk of certain cancers and cardiovascular events, necessitating careful consideration and personalized discussions with a healthcare provider to weigh the benefits against the risks.
Non-hormonal medications
Non-hormonal therapy for menopause presents a range of options for women seeking relief from symptoms without hormone replacement. This approach focuses on managing specific discomforts through various medications and lifestyle adjustments. Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) can address hot flashes and mood swings.
Vaginal estrogen
Vaginal estrogen therapy provides localized relief for menopausal symptoms primarily affecting the vulvovaginal area. Delivered via creams, tablets, or rings, this treatment targets vaginal dryness, itching, and discomfort, as well as urinary symptoms like urgency and frequency. By directly applying low doses of estrogen to the vaginal tissues, it helps restore moisture and elasticity, improving comfort and sexual function. Unlike systemic hormone therapy, vaginal estrogen delivers minimal estrogen to the bloodstream, reducing the risk of systemic side effects. This localized approach is often recommended for women experiencing isolated vulvovaginal symptoms, offering a targeted and effective solution.
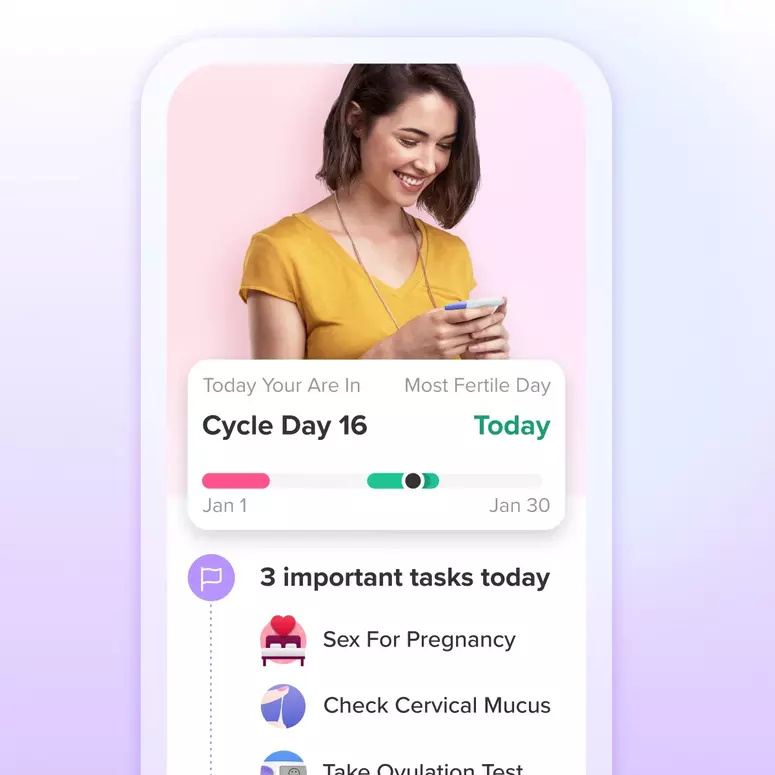
Track your symptoms
Monitoring perimenopause symptoms, such as irregular menstruation, using tools like Glow can empower individuals with a deeper understanding of their body’s changing patterns, potentially mitigating anxiety and stress associated with this transitional phase. Furthermore, maintaining a detailed record of these health patterns provides valuable data for medical consultations, facilitating more informed discussions and enabling healthcare providers to tailor optimal treatment strategies.
Alternative therapies
Supplements for menopause aim to alleviate symptoms through natural or non-hormonal means, though their effectiveness varies and should be discussed with a healthcare professional. Common supplements include black cohosh, which some women use for hot flashes, and soy isoflavones, which contain plant-based estrogens. Calcium and vitamin D are often recommended to support bone health, while magnesium may help with sleep and mood. Additionally, omega-3 fatty acids are explored for potential mood-stabilizing effects. It’s crucial to acknowledge that supplement quality and purity can differ, and individual responses can vary significantly. Due to potential interactions with medications and the lack of rigorous regulation, consulting a doctor before starting any supplement regimen during menopause is essential.