Our Baby Gray Arrived!! Our C Birth Story
💙 Grayson John William
💖 Wednesday 5th August 2020
💚 3.288kg / 7lb 3.5oz
💜 Elective Caesarean birth
My pregnancy had been mostly straight forward, with little to no symptoms for the first trimester. Second trimester I had a negative GD test (woop) and experienced a little PGP, heartburn, and rib pain - at 28 weeks I found out why I had rib pain - baby 'Kiwi' was breech and sitting head up. All was going well and I was hopeful baby would turn by 36 weeks and I could have my dream delivery - a relaxed water birth in a midwife led clinic in our local hospital.
Week 36 midwife appointment, I was sent to the hospital for a presentation scan and to discuss our birth options. The sonographer told me I had polyhydramnios and baby was measuring large: 90th percentile. I'm 5ft and pre-pregnancy weight was 40.5kg.
Breech vaginal delivery was not a recommended birth path as I am a FTM and the hospital do not have specialised staff to support breech birth. Our options were an ECV or elective Caesarean. I chose the ECV and was booked in for the following week.
The next day I get a call and I am told that I've developed GD and needed to be put on Metformin. Baby would need to be delivered at 38 weeks via induction (if the ECV worked) or C birth. Due to Covid, the fact husband couldn't be with me in early labour, debilitating sciatica, go through the discomfort of the ECV and potentially it not work (meaning I would need a Caesarean anyway) and the worry if I needed an emergency C birth after induction then my husband, Tom, could miss our baby's birth, we elected for the planned Caesarean. It was booked for Wednesday 5th August, when I would be 38+3.
I woke up at 4.30am Wednesday full of excitement, anticipation and sciatica. We got to the hospital for 7.30am and we were seen around 8am by the midwives. They informed me that I was booked in for an elective C birth as Kiwi was breech, but they would scan me and if he'd turned then I would instead be sent home and given an induction date.
This is not the same information I was told when I spoke to the obstetrician at 37 weeks, as I specifically asked this question - if he had turned, could I still have the C birth and was told yes. I've got that time slot booked and just to tell them I had prepared physically and mentally for the C birth. The midwives and the surgeon were not happy with this and I was told categorically they would not perform the Caesarean if he had turned. 😫
I then asked if the surgeon could talk me through what he was doing in surgery as per my birth wishes and he said no. That was it. Just no. He was busy operating and needed to concentrate. Thankfully, a midwife called Amanda said she would let me know what was happening at key stages.
They did the scan and he was still breech so at 10am we made our way to theatre.
In theatre, we got to listen to our happy "post baby" playlist as Kiwi was being born. Tom got to cut the cord and we enjoyed skin to skin. It was surreal and beautifulnto finally hold our beautiful Grayson.
After an hour I was wheeled to the post natal ward and had to say goodbye to Tom. All being well, we would be discharged the following day.
However, I spiked a temperature on Wednesday evening, and Gray and I both had to have antibiotics and I was put on a drip.
I struggled to feed Gray as he has significant tongue tie and a tied lower lip (which I am told is quite rare but in the UK we don't do anything about this). We've booked him in on Thursday to get his tongue tie cut and the consultant we spoke to was also amazing at telling me how best to feed him. We'd been trying to cup feed him to avoid nipple confusion and nipple shields on Friday (so he could actually feed on Friday and it felt amazing to be breast feeding him for the first time) but she said no - scratch that, cup feeding is dangerous for tongue tie babies and his suckling would be inefficient and painful (it was). She recommended to bottle feed him expressed milk with Mam bottles as the teat is wide and flat so he will get a good suction. She also gave me advice on pumping as I'd started to become engorged, and if it continued, it meant an even longer stay and potentially more antibiotics and I was not having that. I diligently pumped the engorged boob every hour or so, used cold compresses and double pumped every 3 hours and it cleared up so well.
Gray was really lethargic on Wednesday and Thursday. He also had jaundice, a high haematocrit (thick and sticky blood), added to the fact I couldn't feed him - he vomited back up formula when we tried - he was put on a glucose drip for 3 days.
I felt so useless not being able to care for my baby, but I had a wonderful second time mummy in the bay next to me and her first baby had tongue tie. She told me to ask for a double pump and honestly that was a life saver in the end!
I did not enjoy the postnatal ward, if I'm honest. It was a revolving door of people coming in and out constantly and I could sleep. I had tops of 2 hours between 4.30am Wednesday to 1am Friday and I felt like an emotionally wrung out zombie. I had no schedule for pumping, feeding, sleeping or when I needed my antibiotics and was moved wards 3 times with no warning - I was honestly frazzled and ugly cried.
Wednesday I expressed around 10ml of colostrum for him, but by Thursday (when I was taken off the drip) I was only able to hand express 0.4ml of milk for Gray, and was told he needed a minimum of 37ml every 3 hours. I felt like a failure. Next expression was 3ml, then 10ml and gradually with the use of the pumps, my supply began to increase.
On Thursday evening we were moved from postnatal to TCU, Transitional Care Unit, which is where they look after mostly preemie babies (and one of the only wards where partners could visit!)
I loved TCU and was honestly a little sad when we were discharged!
They were so attentive to me and to Gray, they explained what was going on, as no one had done this in much detail, it was all very vague "Gray has an infection" but didn't say from what/why.
I started to get more of a routine for pumping and Gray's feeding by using an app called Huckleberry. You monitor his feeds, nappies, pumping and sleep. It is amazing.
Despite all his feeding issues, Gray only lost 80g when he was weighed on Saturday. 😁
Tom was able to visit from Friday onwards and this helped me so so so much! Sometimes just little things like getting me a water or cleaning the pumps. Time seemed to fly in there.
Finally, in the early hours of Monday morning, Gray had his final antibiotic dose and his cannula could be taken out.
I was told I should be able to go home that day! Tom arrived at 3.30pm to help me pack and take me home. Gray had been cleared to leave but I just needed the Dr to come and assess me, which one finally did at 10pm(!). Apparently my haemoglobin dropped after the op and it was too low, and my CRP (infection marker) was way too high on Thursday/Friday but no repeat blood had been taken so they had to urgently send one up on Monday afternoon and that came back much lower which was good. I've been on Iron tablets for the low haemoglobin so the Dr asked me a few questions but as I feel fine in myself, no palpitations, dizziness, no shortness of breath we were given the green light to leave at 10.30pm.
Arrived home at 11pm for a feed, nappy change and introduce Gray to our two cats. I took the first bottle feed at 2am and Gray slept until 6am when Tom took over and I could pump.
All in all, we had quite a few hurdles to overcome as a FTM but we've done it and come out the other side stronger for it.
Tom, our families and our hypnobirthing instructor provided me with so much support and they've picked me up at my lowest and now can't wait to see Grayson! 💕
Anyway, that is my story - now for photos!








Let's Glow!
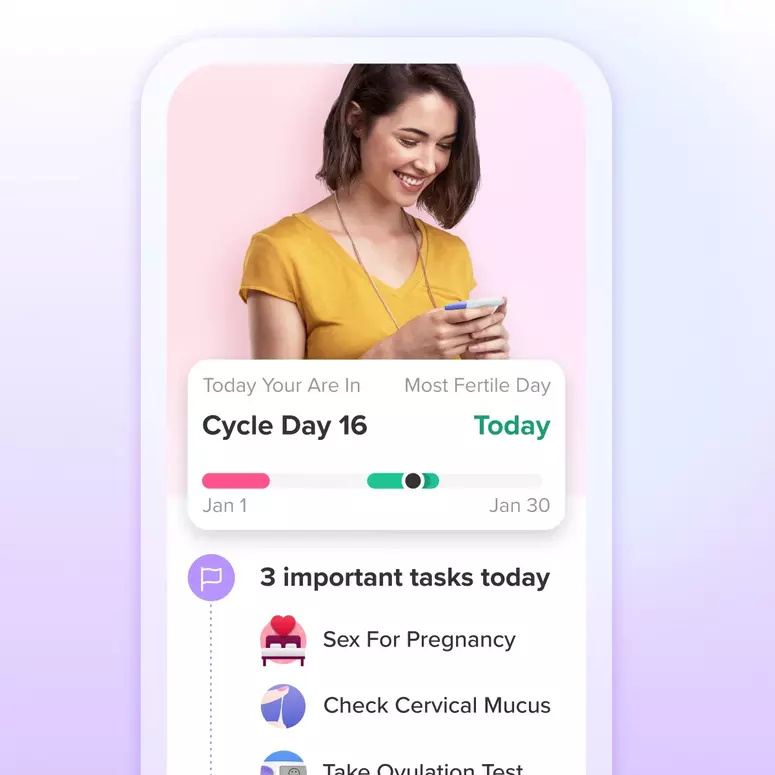
Achieve your health goals from period to parenting.