IVF/Insurance Question
Hi everyone! My husband and I are preparing to start IVF within the next 6 month or so due to my husband having severe male factor infertility. We recently found out that his insurance covers IVF, but my insurance does not. I will not be able to switch to his plan until open enrollment in the fall, which would go into effect January 2022. While I’m VERY grateful his plan covers a lot, I hate to wait until January when I’ve already been waiting for what feels like forever to get started. We started our infertility journey a year ago.
My question is for IVF couples who had two different plans. How did billing work for you? Do you choose whose plan is billed? Or do they bill the person who the procedure is being completed on? For example, I would get billed for meds I take/retrievals/transfers/etc., and my husband would be billed for things specifically related to him? Who gets billed for things that involve both partners, such as genetic testing? I know everyone’s plans are different, but I’m curious how this worked for others.
Thank you!!!
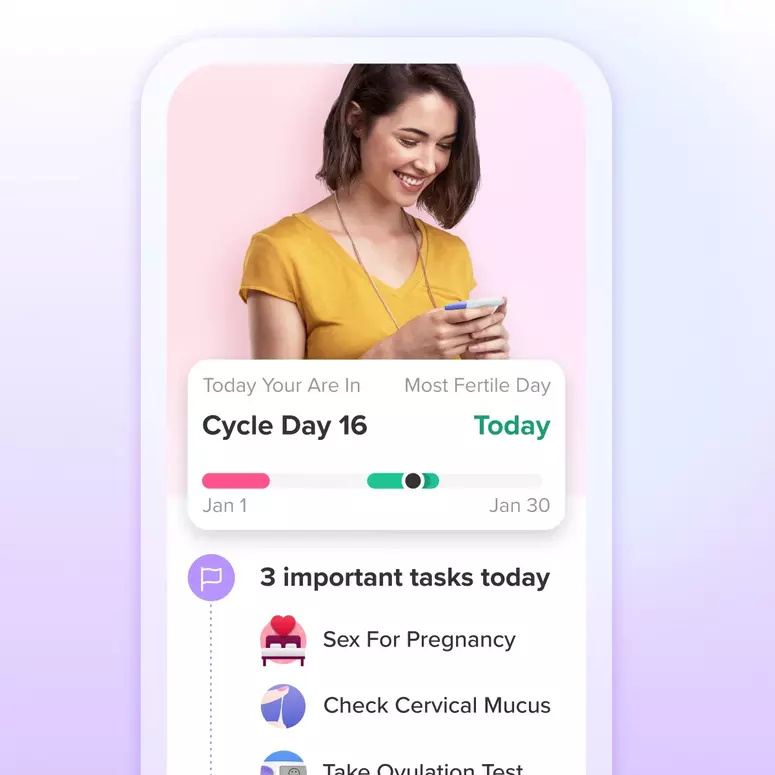
Achieve your health goals from period to parenting.