I don’t have commercial insurance anymore but when I did I think my out of network deductible was $1000. I don’t know what the percentage off I would get if I would have met it. But my therapist does not take our insurance now either (Tricare) so I have to just pay cash. It’s expensive ($150/session) but she’s been my therapist for seven years so I didn’t want to find someone else
Out of Network Billing
Does anyone (in the US) have experience with billing insurance for out of network providers? I’m wanting to start therapy with a therapist that, at least on paper, looks amazing for my situation. But she doesn’t accept insurance. I’m fine paying the out of pocket fees, and my insurance does have an out of network deductible. Would I just send the bills for her to my insurance company and hope to get a small percentage back? I would love any insight or personal experience anyone has.
Cross posting this, because I feel like it could be helpful for more than just my situation.
75
views • 0
upvotes • 5
comments
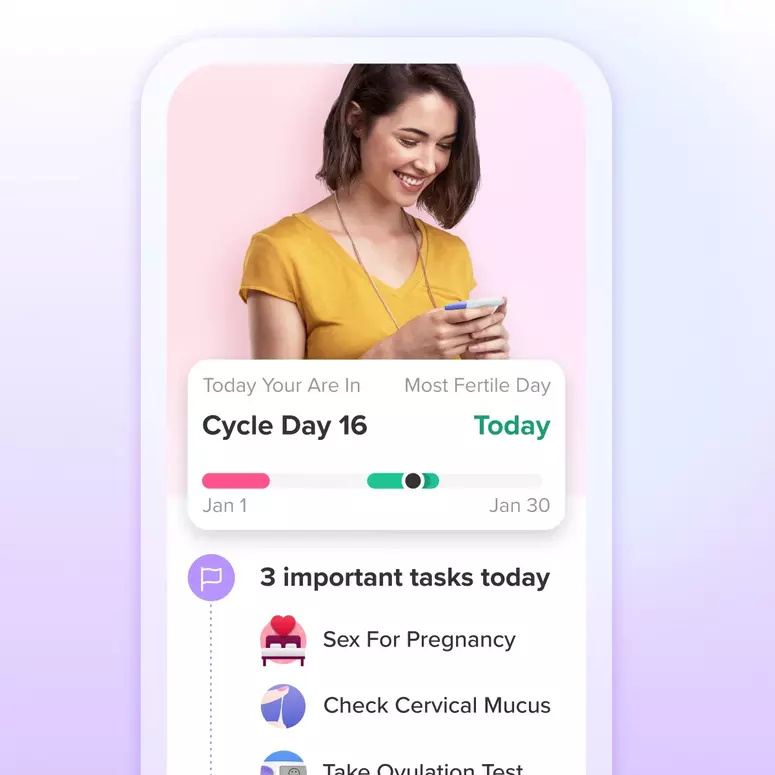
Let's Glow!
Achieve your health goals from period to parenting.