DETAILED FTM VAGINAL BIRTH STORY
I was due May 2nd and my contractions began Friday afternoon (April 27th) after several days of attempting to get labor going with walking, bouncing, and more. Contractions were long and painful but never quite frequent enough for a L&D visit. After some extra spicy Mongolian food (beansprouts instead of noodles, my favorite!) we kept up on our feet as Josh and I ran our last minute errands timing contractions as they came…. every 15 minutes or less, over a minute long each all the rest of the day Friday, Saturday, and Sunday morning.
Sunday Afternoon – April 29th
I was spent, the contractions kept me up all night every night but after a new frustrated calls to L&D throughout the weekend I was told I still wasn’t ready to come in. Our bags were packed and loaded in the truck, the baby room was set up, and everything had been sanitized or Lysol wiped. I made another desperate call in, and was told I could come in to be monitored or given an Ambien to help me get some much needed rest. We went in and I was only 2 cm dilated. I was shocked and felt totally defeated that after all the pain and breathing exercises I was only 1/5th of the way there. Our nurse offered to come back in an hour and see if I would progress enough to be admitted and I leapt at the opportunity. As soon as the door closed behind her I marched, jogged, jumped squatted and rolled my hips as much as I could that whole hour stopping only when the pain was so intense that I’d topple onto the bed. It paid off, when my hour was up our nurse arrived for my check and I was up to 3.5 cm! She got on the phone with the midwife and let her know I was progressing and being admitted. I was so excited that we wouldn’t leave the hospital without our son!
I labored a few more hours in our new room to 5 cm with nothing but Josh, a hot shower, and some Cheez-Its for comfort. I’m so thankful we took the birth class together because everything I’d learned and practiced for this day left me but Josh was there to coach me through each contraction. I still hadn’t slept and was beyond exhausted and only half way through dilation. I moved back over to the bed to labor laying down and with the next shift change of nurses I asked for the epidural. Thankfully, the anesthesiologist was there in minutes and the most painful part was the numbing shot. After two tries and I was ready to nap away the remainder of my labor but not soon after receiving my epidural my contractions were slowing. The doctor on the floor came in and recommended a low dosage of Pitocin to regulate my contractions and keep them coming steadily. I obliged and Pitocin was added to my IV.
As it turns out, it’s pretty hard to sleep when you’re excited to meet your son. When I did finally doze off my nurse ran in and said I needed to turn over NOW. I was flipped onto my stomach, my Pitocin was shut off and an oxygen mask was placed over my face. Two more nurses came in checking the monitors. My baby’s heart rate had dipped but it was moving back up where it needed to be and I was left to continue my nap.
Monday Early Morning – April 30th
I woke up in terrible pain, and could feel my contractions coming; wave after wave after excruciating wave I did my best to breathe my way through. We called the nurse and she said she would send for the anesthesiologist. We waited for 45 minutes. It was agony. Through the pain I did my best to be pleasant to the staff and my husband knowing they were doing all they could to keep me comfortable. My labor playlist played as I breathed though each wave. My anesthesiologist arrived and was there to fix me up again. He administered more medication and said it would be about 15 minutes before it would kick in. We waited but still nothing except more contractions. We called again, he administered more, and we waited. I drew my mind inward to cope with the pain and did what I could to focus on something else. In doing so I looked around the room and noticed a grey wire by my head, it went no where, just the end sitting on soaked sheets. Still in pain, we called again. When my anesthesiologist came back, I asked if the wire should have been connected somewhere. A look of panic crossed my nurses face and I was sat up (surprisingly easy to do after so long without an epidural) and my catheter was reconnected. He manually injected Lidocane directly into my line, administered multiple units of medication, and finally after 20 more minutes I was free from the intense contractions.
I slept another hour and my nurse came in to check me. I was at 9 cm, water had broken at some point, and I was almost ready to push! She turned off my epidural pump and instructed me to call her when I felt constant pressure because it was time to push then. I waited and felt the contractions coming again. Turns out “pressure” and “pain” have two different meanings in L&D. I wasn’t supposed to be in pain… Oops! When the “pressure” was too much we called for the nurse and she checked me again. I was in intense pain and was stuck at 9 cm, swollen due to my baby’s head pressing down onto my cervix. My nurse called my midwife to see what we should do and my very patient anesthesiologist was back in the room delivering enough medication to my epidural space that I was again blissfully unaware of the war raging in my abdomen.
My midwife arrived, it had been so long from when she answered my call to L&D that she had served her full shift, went home, and was back again for another 12 hours. She checked and sure enough I was swollen and no longer progressing. This brilliant woman decided to have me push through the last 1 cm to get my baby through my cervix and it worked! I was allowed to rest while the nurses’ shifts changed and I was introduced to my new nurse who would assist me through pushing my son down while my midwife left to deliver another baby.
My new nurse was wonderful she brought out a mirror for me to see what was happening as I pushed and was incredibly kind. She cheered me on the whole 3 hours of pushing as my son’s head was turned the wrong way and was making it harder to get all the way down. My hospital only allows three hours of pushing before looking at interventions so my nurse texted my midwife to see if forceps or a vacuum might be needed. She was still busy helping bring another life into this world. My nurse asked if I had another 30 minutes left in me or if I wanted to just wait. I took those 30 minutes and gave everything I had until my nurse said STOP. She said I was ready to deliver my baby. My midwife came in and said she never thought she would be delivering my baby when we had first spoke on the phone.
April 30th, 2018 – 10:37 AM
After 3 more pushes Maddox Joshua was placed on my chest. He was 21 inches, 8lbs 2 oz and latched immediately. From the first hard contractions 15 minutes apart to delivery it was 77.5 hours total.
My midwife took care of the aftermath stitching up some minor tearing, pulling out a stuck blood clot, delivering the placenta (and plenty more) then we were rolled into recovery to meet our very excited family.
Less than 2 Hours Old



One Month Old

2 Months Old

3 Months Old

4 Months Old

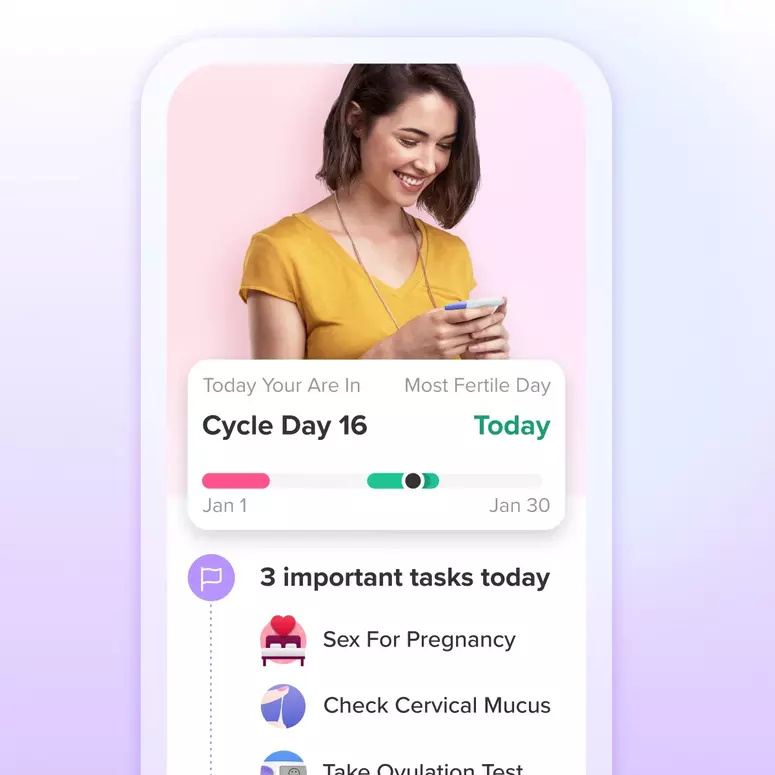
Achieve your health goals from period to parenting.