Subchorionic Hemorrhage: What You Need to Know About Bleeding in Early Pregnancy
Spotting or bleeding during pregnancy can be alarming, and discovering it’s caused by something called a subchorionic hemorrhage won’t do much to ease your anxiety.

While subchorionic hemorrhages sound scary, most often, they resolve on their own. Still, bleeding or spotting during pregnancy is nothing to sleep on, and you should definitely report it to your doctor.
In this article, we’ll dig into what a subchorionic hemorrhage is and what it means for your pregnancy.
What is a subchorionic hemorrhage?
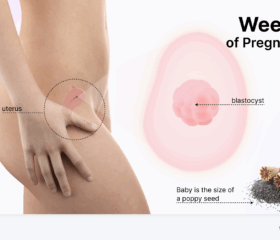
A subchorionic hemorrhage (also called a subchorionic hematoma or subchorionic bleed) is when blood collects between your uterine wall and the chorion.
The chorion is the outer membrane that surrounds your baby in the womb. As your pregnancy progresses, it will form the placenta. However, sometimes, instead of remaining in place and behaving itself, it will detach from the wall of your uterus. When that happens, it bleeds, forming a subchorionic hematoma. 1
Subchorionic hemorrhage is a pregnancy complication, but a very common one. By some estimates, this causes approximately 11% of all cases of vaginal bleeding between week 10 and week 20 of pregnancy, making it one of the more common causes. 2
The good news is that most subchorionic hemorrhages resolve on their own and don’t cause any long-term problems.
Subchorinic hemorrhage is different from placental abruption
The placenta—the organ that the chorion will eventually form—can also prematurely separate from your uterus, causing some bleeding. This is known as placental abruption, and it usually happens later in pregnancy than a subchorionic hemorrhage (20 weeks and after). Unfortunately, if you’ve had a subchorionic hematoma, that puts you at a significantly higher risk of experiencing placental abruption.
What causes a subchorionic hemorrhage?
Doctors often can’t pinpoint the exact causes of a subchorionic hemorrhage, and it seems to frequently happen spontaneously.
However, certain factors may increase your risk: 1
- IVF pregnancies: If you get pregnant by using in vitro fertilization (IVF), you may be more likely to have a subchorionic hemorrhage.
- Uterine abnormalities: If you have certain structural issues with your uterus, that could put you more at risk of a hemorrhage.
- History of miscarriage: Women with a history of recurrent miscarriages may have a higher risk. 2
- Other risk factors: High blood pressure and certain drugs may also increase your risk. 3
What are the symptoms of a subchorionic hemorrhage?
Many women with a subchorionic hemorrhage don’t experience any symptoms at all. However, the most common symptom is vaginal bleeding or spotting. This may affect the color of your pregnancy discharge, causing it to turn brown, pink, or red. Some women may also experience mild abdominal cramping or pain. 2
Because bleeding and cramping during pregnancy can signal several different complications (and sometimes doesn’t signify anything at all), get in touch with your doctor if you experience these symptoms. When you’re expecting a child, you don’t want to self-diagnose—it’s better to get yourself seen.
How is a subchorionic hemorrhage or hematoma diagnosed?
If you have symptoms (bleeding) that suggest you have a subchorionic hemorrhage, a pregnancy ultrasound will determine what’s causing it. That will also let your doctor check on your baby’s well-being, measuring her heartbeat and ruling out more serious conditions, like a miscarriage.
What are the potential risks of a subchorionic hemorrhage?
Most subchorionic hemorrhages resolve on their own, and it’s possible that, having had one, you’ll go on to have a perfectly healthy and normal pregnancy.
However, this condition is correlated with an increased risk of developing further complications, such as: 4
- Miscarriage: Larger hemorrhages, particularly those greater than 25% of the gestational sac size, have been associated with an increased risk of pregnancy loss. 2 If you have a larger hemorrhage, your doctor might categorize your pregnancy as a threatened miscarriage (i.e., a higher-risk pregnancy that requires more medical attention).
- Preterm labor and other complications: Having a subchorionic hemorrhage may put you more at risk of preterm labor and the premature rupture of membranes (PROM). It may also influence your odds of developing pregnancy-induced hypertension later in the pregnancy. 2
- Placental abruption: There’s a slightly increased risk of the placenta separating from the uterine wall later in pregnancy. 2
The risk of developing these conditions is relatively low, and again, most women with subchorionic hemorrhages go on to have viable pregnancies. Larger subchorionic hematomas are connected with greater risks, whereas smaller bleeds usually aren’t as big a deal. 2
How to treat and manage a subchorionic hemorrhage
In most cases, there’s no treatment required for a subchorionic hemorrhage because they typically dissolve on their own. How long this will take depends on the size of the hemorrhage, but once other conditions are ruled out, the usual approach is simply to wait and see:
Your doctor may recommend pelvic rest, which means avoiding sex during pregnancy (as well as strenuous activities in general). They probably won’t recommend strict bed rest, as it hasn’t been shown to improve outcomes (and, in fact, can actually lead to the development of blood clots in your legs). 5 Either way, it’s best to defer to your doctor’s advice, but feel free to ask as many questions as you like.
Your healthcare provider will likely schedule follow-up ultrasounds to monitor the size of the hemorrhage and check on your baby’s development. 4
Immunoglobulin injections
In some cases, you may be given a RhoGAM shot, which contains immunoglobulin. This is provided if your blood is Rh-negative but your baby’s blood is Rh-positive. This is a preventative injection to stop your immune system from treating the baby’s blood cells like an infection and is not a treatment for subchorionic hemorrhage itself. 6 2
Can you prevent subchorionic hemorrhage with at-home remedies?
No—it’s important to note that there are no natural remedies or supplements proven to prevent or treat subchorionic hemorrhage.
Moreover, many natural or homeopathic remedies have not been evaluated by the FDA, and regardless, you shouldn’t introduce any new supplements to your body during pregnancy without consulting with your doctor.
What to do while you wait for your subchorionic hematoma to resolve
While it may be comforting to know that most subchorionic hemorrhages resolve on their own, the waiting isn’t always so easy.
Your best course is to focus on business as usual. Eat a balanced pregnancy diet (look into which foods to avoid during pregnancy), keep taking your prenatal vitamins, and stay hydrated.
Above all, try not to panic. Anything involving internal bleeding can be distressing (for obvious reasons), but most of the time, this is a relatively minor condition and not an emergency.
When to seek medical attention
Your doctor will keep a close eye on you after catching a subchorionic hemorrhage, but you should seek further medical attention immediately if: 7
- Your bleeding increases
- You’re passing tissue from your vagina
- Your pain or cramps get worse
- You feel faint or dizzy
- You have a fever or chills
All of these are the classic signs of a miscarriage. Don’t hesitate to get in touch with your doctor right away.
Final thoughts
There’s no shortage of things that can send your anxiety through the roof when pregnant. Hearing the words “subchorionic hemorrhage” certainly won’t do much to ease your worries.
Thankfully, this complication will probably clear up by itself without causing any long-term harm. Just stay in touch with your doctor, keep an eye on your symptoms, and attend your check-ups. You’ll probably be fine.
Article Sources
- Cleveland Clinic. "Subchorionic Hematoma" Retrieved May 2, 2025.
- StatPearls. "Subchorionic Hemorrhage" Retrieved May 2, 2025.
- San Diego Perinatal Center. "Subchorionic Hematoma" Retrieved May 2, 2025.
- Cleveland Clinic. "Subchorionic Hematoma" Retrieved May 2, 2025.
- Baylor College of Medicine. "Maintaining a healthy pregnancy" Retrieved May 2, 2025.
- MedlinePlus. "Rh incompatibility" Retrieved May 2, 2025.
- Johns Hopkins Medicine. "Miscarriage" Retrieved May 2, 2025.