TABLE OF CONTENTS
What is PMS?
Premenstrual syndrome (PMS) is a combination of symptoms that many women get about a week or two before their period. According to the Office on Women Health (https://womenshealth.gov/), as many as three in four women say they get PMS symptoms at some point in their lifetime. Most women, over 90%, say they get some premenstrual symptoms, such as bloating, headaches, and moodiness. For some women, these symptoms may be so severe that they miss work or school, but other women are not bothered by milder symptoms. On average, women in their 30s are most likely to have PMS.1
What are the symptoms of PMS?
PMS symptoms are different for every woman. Your symptoms may also change throughout your life. PMS can be both emotional and/or physical, but some common symptoms include:1
- Cramps: Painful muscle contractions in the uterus, often felt in the lower abdomen, which can range from mild to severe.
- Mood swings: Rapid and unpredictable shifts in emotional state, including irritability, sadness, or sudden outbursts.
- Swollen or tender breasts: Increased breast tissue sensitivity and swelling due to hormonal fluctuations.
- Tension or anxiety: Feelings of unease, worry, or nervousness, sometimes accompanied by physical symptoms like restlessness.
- Headache or backache: Pain in the head or lower back, often attributed to hormonal changes and muscle tension.
- Sleep problems (sleeping too much or too little): Disruptions in sleep patterns, leading to either excessive drowsiness or insomnia.
- Changes in appetite: Fluctuations in hunger, including increased cravings or a decreased desire to eat.
- Less interest in sex: A reduced libido or sexual desire, potentially linked to hormonal shifts and physical discomfort.
Why do you get PMS?
While the exact cause of PMS remains unclear, scientific research points to a few key theories. Many experts believe that the cyclical fluctuations of the hormones estrogen and progesterone throughout the menstrual cycle play a significant role. During the luteal phase after ovulation, these hormones peak and then rapidly decline.2 This hormonal shift is thought to trigger various PMS symptoms, including anxiety and irritability, due to their influence on brain chemistry and other bodily functions
Additionally, changes in brain chemistry, specifically involving neurotransmitters like serotonin and norepinephrine, are considered a contributing factor. 2 A drop in estrogen levels may lead to the release of norepinephrine, subsequently affecting the production of dopamine, acetylcholine, and serotonin. These neurochemical changes can manifest as sleep disturbances and a lowered mood. Furthermore, individuals with pre-existing mental health conditions like depression or anxiety may be more susceptible to experiencing PMS or its more severe form, PMDD.3 A family history of mood disorders can also increase this risk.4 Lifestyle factors such as smoking, a diet high in unhealthy fats, sugar, and salt, lack of exercise, and poor sleep quality are also believed to potentially worsen PMS symptoms.5
How is PMS diagnosed?
Diagnosing PMS isn’t about a blood test or scan. It comes down to understanding your personal experience. Your doctor will really focus on the pattern of your symptoms – when they show up and how much they impact your daily life.
You’ll likely be diagnosed with PMS if your symptoms consistently appear in the five days leading up to your period for at least three menstrual cycles in a row, and then ease up within about four days after your period begins. Importantly, these symptoms will be significant enough to interfere with your usual activities and enjoyment of life.
Keeping a detailed record of your PMS symptoms for a few months is super helpful for your doctor. Jotting down each day which symptoms you’re experiencing and how intense they are, whether on a calendar or using an app on your phone, can reveal clear patterns. Bringing this log with you to your doctor’s appointment will give them valuable insight to make an accurate assessment.
Managing PMS
Dietary Adjustments
Nourishing your body with whole foods like fruits, vegetables, and whole grains is a foundational step in easing PMS symptoms, as they provide essential nutrients and fiber that support overall well-being. Conversely, it can be beneficial to limit your intake of processed foods, caffeine, and alcohol, as these substances can sometimes worsen symptoms such as bloating, mood swings, and sleep disturbances. Staying well-hydrated by drinking plenty of water is also crucial, as it can help to reduce bloating and combat fatigue. Some research suggests that ensuring adequate intake of calcium and vitamin D may also play a role in alleviating PMS discomfort, although it’s always wise to discuss supplementation with your doctor to determine what’s right for you. Finally, incorporating magnesium-rich foods like leafy greens, nuts, and seeds into your diet may offer relief from muscle cramps and contribute to a more stable mood during your cycle.
Stress Management Techniques
Incorporating gentle physical activities like yoga or stretching into your routine can be incredibly beneficial for easing the physical discomfort of PMS by releasing muscle tension and promoting overall relaxation. Beyond physical ease, making a conscious effort to spend time in nature has been shown in studies to have a positive influence on mood, offering a sense of calm and well-being. Furthermore, don’t underestimate the power of engaging in hobbies and activities that bring you joy. Setting aside time for these enjoyable pursuits can serve as a welcome distraction from PMS symptoms and provide a significant boost to your emotional state during this time.
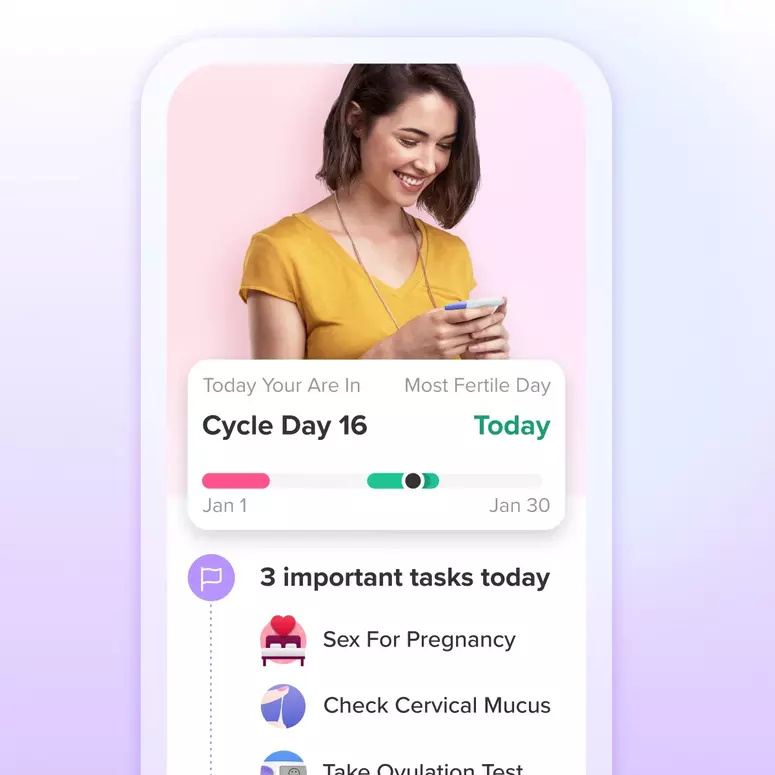
Track your cycle
Tracking your cycle can also really help you understand and manage your symptoms. Apps like Glow make this easy, offering mobile tracking, personalized PMS alerts, and the ability to log symptoms like pain and mood changes, which can help you spot patterns from cycle to cycle.
Medical treatments
Over-the-counter pain relievers, such as ibuprofen, naproxen, and aspirin, can alleviate physical PMS symptoms like cramps, headaches, backaches, and breast tenderness. Some women find that preemptive use, starting just before menstruation, can minimize pain and bleeding.1
For those experiencing inadequate relief from over-the-counter options, prescription medications may be considered. Hormonal contraceptives, including birth control pills, can regulate hormone levels and reduce PMS symptoms. In severe cases of mood-related symptoms, selective serotonin reuptake inhibitors (SSRIs) may be prescribed. While some studies suggest potential benefits from calcium, magnesium, and vitamin B6 supplements, consultation with a healthcare professional is essential before initiating any supplement regimen.1
Herbal supplements
Many women have found comfort from PMS symptoms through practices like yoga and meditation, which can help to soothe both the physical and emotional aspects of PMS. Additionally, some explore herbal supplements for relief. However, it’s absolutely crucial to have a conversation with your doctor or nurse before starting any herbal supplement. This is because these supplements can potentially interact with other medications you might be taking, which could either reduce the effectiveness of your other medicines or even lead to dangerous side effects.1 While some research studies suggest that certain herbal supplements may offer relief from PMS symptoms, the findings are not always consistent across different studies. It’s also important to be aware that many herbal supplements should not be combined with other medications. Some of the herbal supplements that women sometimes use to ease PMS symptoms include black cohosh,6 often used for menopausal symptoms but also tried for PMS relief; chasteberry,7 which some women take in liquid extract or pill form for PMS, but it’s important to note that it should not be used by those on hormonal birth control or hormone therapy; and evening primrose oil capsules, which some women find helpful, although research on its effectiveness for PMS has yielded mixed results. Prioritizing your safety by discussing any potential supplements with your healthcare provider is always the best approach.
Final thoughts
Medical advice should be sought when PMS symptoms significantly disrupt daily life. A healthcare provider can determine the most appropriate treatment plan and rule out underlying medical conditions.
Article sources:
- Office on Women’s Health. Premenstrual syndrome (PMS). Retrieved February 3, 2025.
- Mayo Clinic. Premenstrual syndrome (PMS). Retrieved Feb 25, 2022
- Cleveland Clinic. Premenstrual Dysphoric Disorder (PMDD). Retrieved February 02, 2023
- University of Rochester Medical Centre. Premenstrual Dysphoric Disorder (PMDD) Retrieved February 25, 2022
- Thiyagarajan DK, Basit H, Jeanmonod R. Physiology, Menstrual Cycle. Retrieved 2024 Sep 27
- Dietz, B. M., Hajirahimkhan, A., Dunlap, T. L., Bolton, J. L. (2016). Botanicals and their bioactive phytochemicals for women’s health. Pharmacological Reviews, 68(4): 1026-1073
- Cleveland Clinic. What Is Chasteberry, and What Can It Do? Retrieved November 22, 2022